Portable radiography systems redefining PoC imaging and mobile diagnostics.
As imaging continues to advance through innovations such as photon-counting CT, improved detectors, and AI-driven workflows, radiography is also experiencing a quieter but equally important shift toward portability. At RSNA 2025, a clear trend emerged: manufacturers across Asia, Europe, and North America are accelerating development of ultra-portable and hybrid-portable X-ray systems designed to bring imaging closer to the point of need.
For years, “portable X-ray” meant large mobile carts rolling through hospitals and long-term care facilities — essential tools but fundamentally tied to institutional, in-facility workflows. What is emerging is materially different: lightweight generators, compact foldable carts, “X-ray in a box” kits, and even handheld CNT-based devices capable of delivering essential imaging outside the walls of traditional radiology departments.
These systems do not—and cannot—replace full radiography rooms. However, they meaningfully expand the range of clinical environments where diagnostic imaging is feasible. From TB screening programs and rural outreach to home-based care, mobile clinics, and rapid-response scenarios, ultra-portable X-ray is quietly reshaping the geography of radiology.
As this category expands, clarity becomes increasingly important. Vendors frequently use terms such as portable, mobile, field-ready, and fully diagnostic interchangeably, even though the systems presented at RSNA varied by more than an order of magnitude in weight and tube power—and, consequently, in clinical capability.
To bring clarity to this evolving landscape, this article introduces a two-dimensional classification framework that distinguishes what each system is (its technical architecture) from what it can reliably do (its clinical imaging capability). Grounded in radiographic physics and aligned with ACR/AAPM technique standards, this framework provides consistent way to interpret the ultra-portable X-ray market today—and to understand the practical limits and future direction of point-of-care and mobile radiography.
What RSNA 2025 Reveals About Ultra-Portable X-Ray (Key Insights)
Before introducing the classification framework and reviewing the manufacturers whose booths I visited at RSNA, it is worth stepping back to highlight several key insights about the ultra-portable X-ray market, as revealed by what was on display at the meeting.
From Observations to Framework
Taken together, these observations point to a common conclusion: ultra-portable X-ray is no longer a single category, but a structured ecosystem shaped by both physical design choices and immutable radiographic constraints. To move beyond general impressions and marketing claims, a more precise vocabulary is needed—one that distinguishes how systems are architected from what they can reliably image. The sections that follow introduce a structured framework that separates Technical Architecture Classes from Clinical Capability Classes, providing a consistent basis for comparing the systems presented at RSNA and for interpreting the vendor landscape that follows.
Technical Architecture (TAC-I to TAC-III)
Ultra-portable X-ray systems differ not only in clinical capability, but in how they are physically constructed, powered, and deployed. To make meaningful comparisons across devices, it is useful to first distinguish their technical architecture—the way the generator, tube, detector, support structure, and power systems are combined into a usable platform. The Technical Architecture Classes (TAC) introduced below separate hand-carried generators, integrated portable DR kits, and compact cart-based systems, providing a structural framework that explains why devices with similar clinical claims can differ substantially in weight, setup complexity, and real-world deployability.
Technical Architecture Classes
TAC I — Portable Generators (Hand-Carry Class)
They represent true ultra-portability and are widely used in TB programs, humanitarian missions, and basic mobile imaging. These are the smallest and lightest radiography systems:
- Handheld CNT emitters
- 5–12 kg HF generators
- Minimal or optional stands
- Paired with a separate DR detector and console
TAC-II — Integrated Portable DR Kits (“DR in a Box”)
These systems are well-suited to traveling clinicians, home visits, mobile vans, and rural outreach. A step above TAC-I in integration and workflow readiness:
- Generator + detector + workstation packaged into cases
- May include small or foldable stands
- Designed to be transported in a car or carried by small teams
- Faster setup, unified acquisition workflow
TAC-III — Compact Portable Carts (Foldable / High-Output)
These are the only portable systems capable of limited abdominal imaging and approach partial general radiographic capability in non-obese patients. Not full hospital mobile carts—but lighter, foldable systems with:
- 4–8 kW HF generators
- Tube arms offering stability and positioning control
- Support for grids
- More robust exposure performance
Please note that several TAC-III systems presented at RSNA share closely aligned hardware architectures, reflecting a broader industry trend toward common OEM platforms with differentiation occurring at the system integration and workflow level.
Clinical Capability (CC-I to CC-VI)
A summary of the clinical capability scale, included below, is built on radiographic physics, including kVp/mAs ranges, tube current, exposure time, SID, and patient habitus. This scale is vendor-agnostic and aligned with ACR/AAPM technique expectations. For a complete view click on the image.
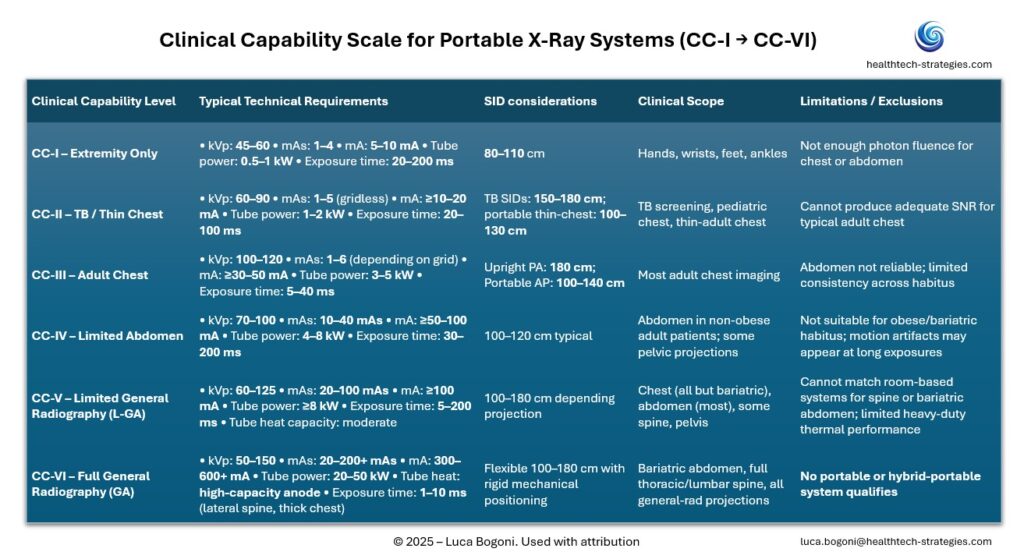
Clinical Capability Classes
CC-I — Extremity-Only
> 45–60 kVp, very low mAs, no grid, short SID.
> Applications: hands, feet, small joints.
CC-II — TB / Thin-Chest
> 60–90 kVp, gridless 1–5 mAs, 100–130 cm SID (150–180 cm in screening vans).
> Applications: TB outreach, pediatrics, thin adults.
CC-III — Adult Chest
> 100–120 kVp, 1–6 mAs, ≥30–50 mA, 100–180 cm SID.
> Applications: standard thoracic radiography.
CC-IV — Limited Abdomen
> 70–100 kVp, 10–40 mAs, ≥50–100 mA, grid recommended.
> Applications: non-obese adult abdomen, pelvis, some spine.
CC-V — Limited General Radiography (L-GA)
> Approaching room-like capability but still limited by power, tube heating, and stand rigidity.
> Applications: most non-bariatric chest/abdomen, some spine.
CC-VI — Full General Radiography (GA)
> 20–50 kW systems with high-heat tubes and 1–10 ms exposures.
> No portable X-ray system reaches CC-VI—a crucial point revealed by the framework
Representative Ultra-Portable X-Ray Systems at RSNA 2025
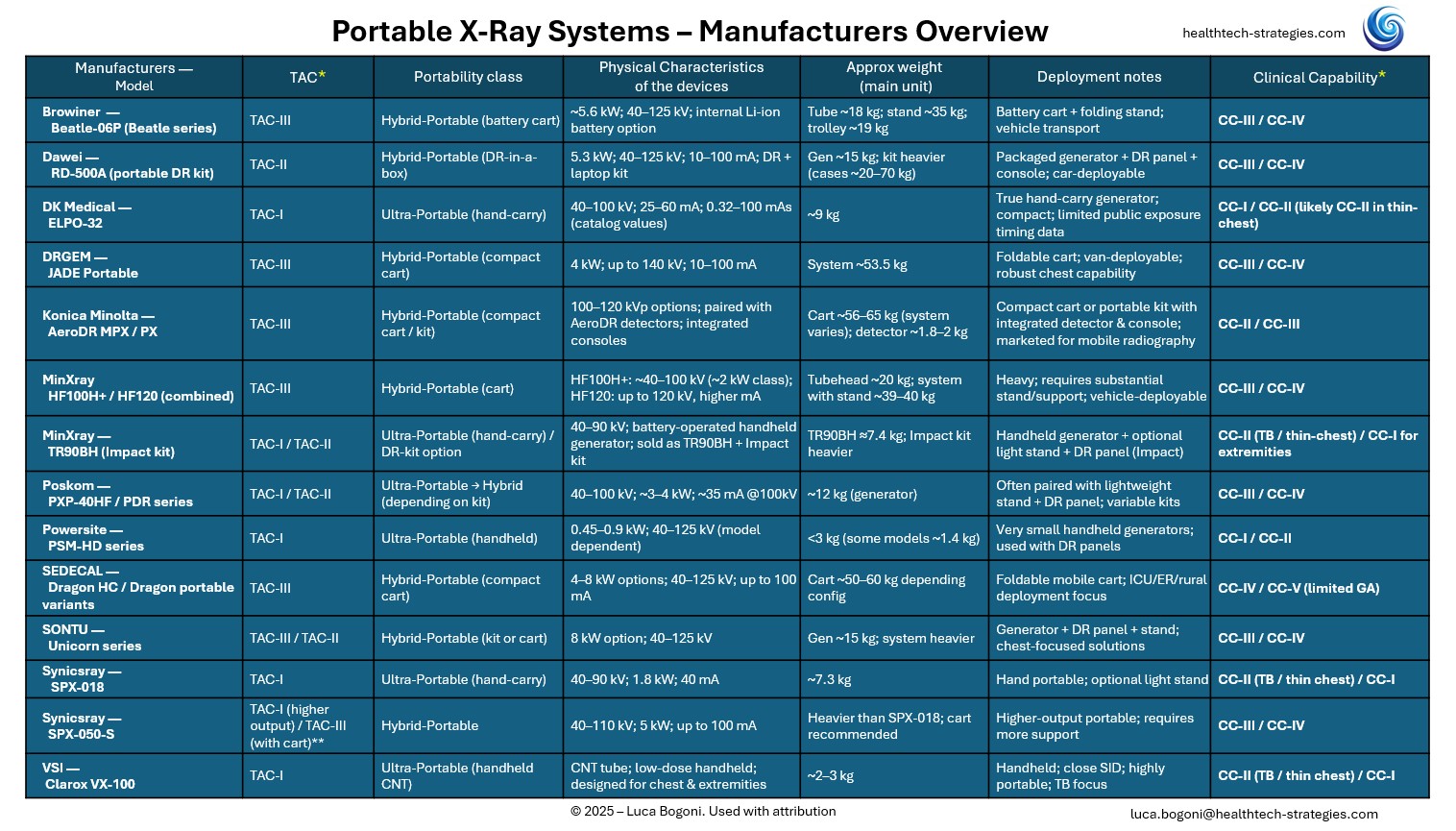
To help readers navigate the rapidly expanding landscape of ultra-portable X-ray systems, we compiled a comparative table of 12 representative vendors showcased at RSNA 2025. These systems span a wide range of technical architectures—from handheld generators to integrated portable DR kits and compact foldable carts—and differ substantially in their real clinical capability.
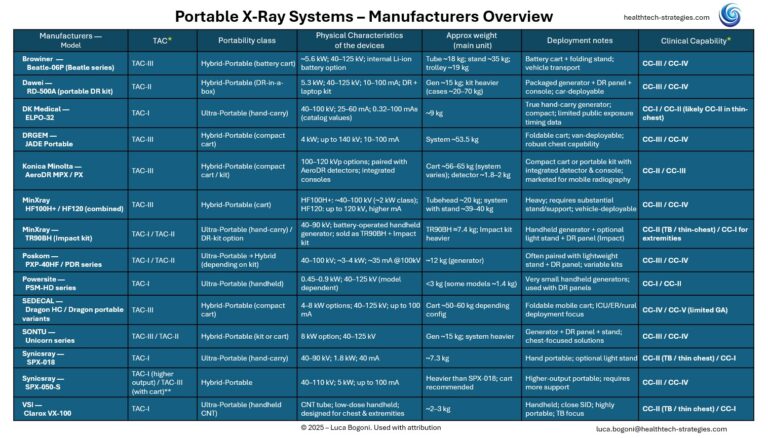
Using the TAC (Technical Architecture Class) and CC (Clinical Capability) framework introduced in this article, the adjacent table provides a structured way to understand where each device fits along the spectrum from extremity-only imaging to limited general radiography. More details on each of these vendors is provided below
Manufacturers Spotlights (Representative Systems at RSNA 2025)
Conclusions: Portable X-Ray Comes of Age—With Clear Boundaries
RSNA 2025 marked a turning point for portable radiography—not because a single breakthrough device emerged, but because the category itself has matured into a clearly stratified ecosystem. Ultra-portable X-ray is no longer a vague promise of “imaging anywhere”; it is a set of well-defined architectures with equally well-defined clinical ceilings.
By separating technical architecture from clinical capability, the TAC × CC framework makes the practical limits of portable radiography explicit. Handheld and luggable systems are well suited to extremity imaging and TB screening; transportable DR kits extend reliable imaging into adult chest and selected abdominal applications; and compact cart-based platforms represent the upper end of portability, approaching limited general radiography in non-obese patients. Full general radiography, however, remains—by necessity—the domain of fixed installations.
This distinction is not a limitation of the framework but its primary value. It enables clinicians, health systems, and program designers to align technology choices with real clinical needs rather than aspirational specifications. At the same time, it highlights where meaningful innovation is still possible: improving efficiency, workflow, and deployability within the CC-III and CC-IV range, rather than attempting to force room-equivalent performance into form factors that physics will not support.
Portable X-ray has already demonstrated its value in global health and community screening. The next phase will be defined not by exaggerated claims, but by thoughtful alignment between physics, clinical need, and care delivery models. RSNA 2025 showed that this alignment is finally taking shape.
Portable X-ray is not just equipment, but infrastructure for distributed care.
Disclosure: This analysis reflects the author’s independent perspective based on publicly available information and observations from RSNA 2025. It is not affiliated with, sponsored by, or endorsed by any manufacturer referenced in the article.